As you have read in my last blog, we know that diets don’t work and that we have plenty of evidence to show us this. But when we go to the doctors, weight loss is usually touted as a cure. You go on the NHS website, most things say that fatness is a cause for many illnesses and weight loss is part of the cure. Why are we still being told to lose weight if they don’t work anyway? You may worry about your health because of being fat/large bodied because that is everything the NHS/doctors/media is telling us constantly. I am free to tell you, it is more complicated that that.
The Connection Between Health and Weight
Weight Centric vs Weight Inclusive?
The first reason is due to the connection between health and weight. The evidence we have shows that there is a correlation between health and weight. It is undeniable, unfortunately. But does that mean that being fat causes ill health and chronic conditions? No. Just that they are related and we do not actually know how they are related. We can really only have theories. The main theories that are shared is what we call “weight centric” which centers weight as important and therefore intentional weight loss as important for health. This is the main system we have experienced across the world in health care for a long time. Which also has been shown to not actually work because dieting and weight loss does not work for the majority of people.
The alternative system is “weight inclusive”. This is where we approach overall “health” more holistically. I know, it sounds a bit “woo woo.” But I promise you that considering someone’s access to healthy behaviours and trying to remove barriers to those behaviours over shaming someone into losing weight is far more beneficial.
Is it the Fat itself? Or Could the correlation be something else?
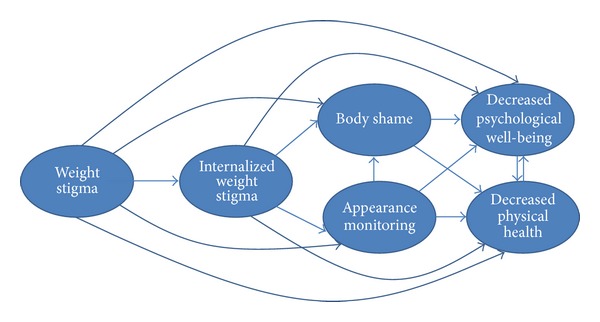
We have studies that show that the experience of weight stigma and weight discrimination causes increased stress, unhealthy eating behaviours, avoidance of physical activity, and psychological issues like depression and low self-esteem (Puhl et al, 2007). Weight stigma and discrimination also may cause weight gain (which isn’t inherently bad it is just something that happens). If we had a systematic change to weight inclusive care, we would still have fat people, but that wouldn’t matter; because all people of any size would receive the healthcare they need.
And is it as easy as receiving healthcare? Yes. The common correlations we have with health and fatness are: –
- Cardiovascular disease
- Type 2 diabetes
- Some cancers
- Joint problems
Weight Stigma and Weight Cycling
These are usually the reasons why people tell me they are losing weight for their “health”. I always think to myself; what happens when you lose the weight and rebound (regain the weight again). Because that is the typical cycle we are looking at. Weight cycling or yo yo dieting. Shall we start the cycle again or break the cycle for good? We cannot ignore the potential risk in weight cycling. There is research to show that weight cycling increases risk of cardiovascular disease as well as type 2 diabetes. We are talking about studies within the last 3 years which have been looking at this.
Cortisol and Weight cycling
With the current wellness trends focusing on cortisol (your stress hormone), it seems like cortisol is far more complex than social media is showing (no surprises there to be honest). When you weight cycle, there is evidence that in the short term, your cortisol increases and over the long term, you may change the way your body deals with cortisol which is not good.
Cortisol, weight and cancer
This increase in cortisol is a mechanism that in theory may actually increase the risk of developing various cancers as well. The links between stress, cortisol and cancer is well known but unfortunately, there are not many cancer and weight stigma papers to be able to say that there is enough evidence to confirm this correlation. I still think it is important to mention. We do have papers to show that experiencing weight stigma increases a specific inflammation marker correlated with increasing some cancers risk.
Weight stigma and cancer
We already know (and many of us fat people have already experienced) that fatness means a completely different kind of doctors appointment, usually with weight loss being the advise for a range of symptoms and people coming away feeling ashamed. This is well documented to put a barrier in the way of fat people going to see the doctor in the first place for any symptoms, but also increases the doctors anti fat bias which in turn means that doctors are more less likely to physically examine a fat person and more likely to dismiss a fat persons symptoms. This form of weight stigma may also increase the risk of developing cancers.
Weight stigma, weight cycling an Cardiovascular disease
Cardiovascular disease is often touted as one of the biggest risks associated with being fat, but what’s not often discussed is how weight cycling and weight stigma play into this narrative. When we talk about weight cycling, we’re talking about the repeated loss and regain of weight that many people experience when they engage in dieting. This constant yo-yoing doesn’t just mess with your metabolism—it also takes a toll on your heart.
Studies have shown that weight cycling is linked to increased risk of cardiovascular disease, not because of fatness itself, but because of the strain that repeated weight loss and regain places on the body. And then there’s weight stigma, which only adds fuel to the fire. The stress and anxiety of living in a society that constantly shames fat bodies can lead to higher cortisol levels, inflammation, and yes, even an increased risk of heart disease. So when we’re told to lose weight for our heart health, it’s worth questioning whether the cycle of dieting and the stigma that comes with it might be doing more harm than good.
Weight stigma, weight and joints
The experience of weight stigma is also correlated with pain sensitivity unfortunately. If you are someone who experiences weight stigma, you are more likely to have a lower threshold for pain including in your joints. The inflammatory markers that I explained are increased with weight stigma may also be responsible for the inflammation related to osteoarthritis. Weight cycling has also been shown in increasing these inflammatory factors as well as the physical mechanism of weight fluctuating and potentially damaging joint cartilage. Weight cycling also comes together with muscle loss which may also be a mechanism that increases pain in the joints.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4132299/
Don’t these sounds so similar to being told that being fat causes all these things. When actually, our bodies are not as simple as this weight centric approach. The weight centric approach allows healthcare professionals to actively harm their patients through weight stigma and then the responsibility for the ill health falls to the individual because society says that fatness is all the individuals fault as weight loss is so easy (I am rolling my eyes because its not easy and once again doesn’t work). But as you can see, being told to diet again and again with the inevitable weight regain afterwards coupled with the experience of weight stigma may actually cause the same risk factors as the weight centric approach says that the fat itself causes. So yes, fatness and health may be correlated but not how we are told.
The Benefits of a Weight Inclusive Approach
Taking a closer look at a weight inclusive approach as see what evidence we have about health and healthy behaviours regardless of weight change, so completely decentering the importance of weight. In research this is also called a Health at Every Size approach which was popular up to about 2 years ago when a researcher who ended up well known for their work with HAES ended up harming the black and fat community.
Weight Inclusive care and type 2 diabetes
We have evidence to show that type 2 diabetes management can be improved regardless of weight change. This evidence can even be found in the same research that the NHS is using to push this soup diet for type 2 diabetes “remission”. The original Diabetes Prevention Program in 2002 showed that exercise, managing stress, being mindful of nutrition were things that significantly reduced risk even with 56% of people not losing weight. We see the same in the Look Ahead study where a secondary analysis showed that nutrition and exercise regardless of weight change actually made better blood pressure control, improved cholesterol levels, and reduced need for diabetes medications.
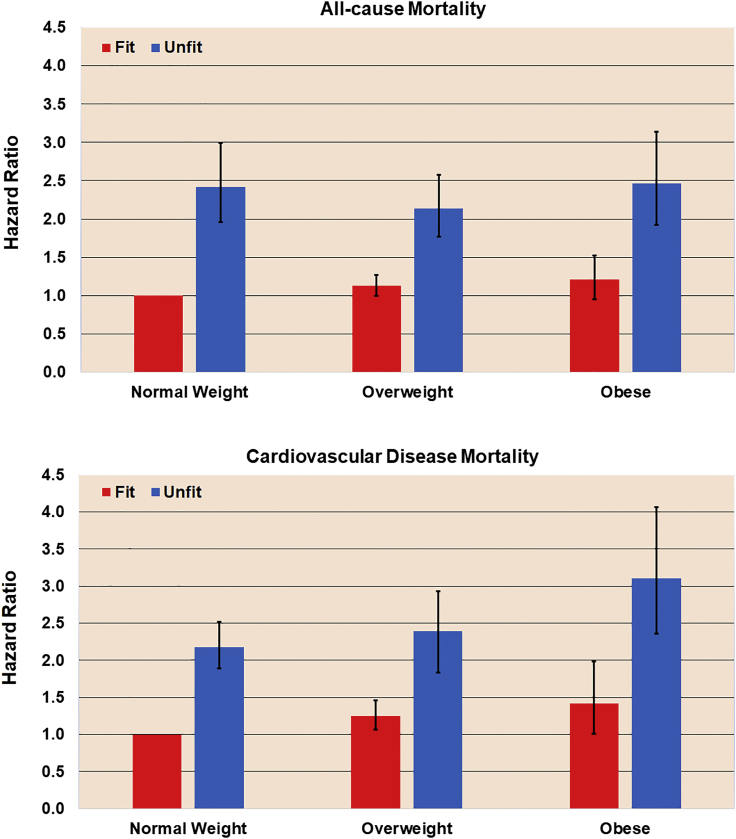
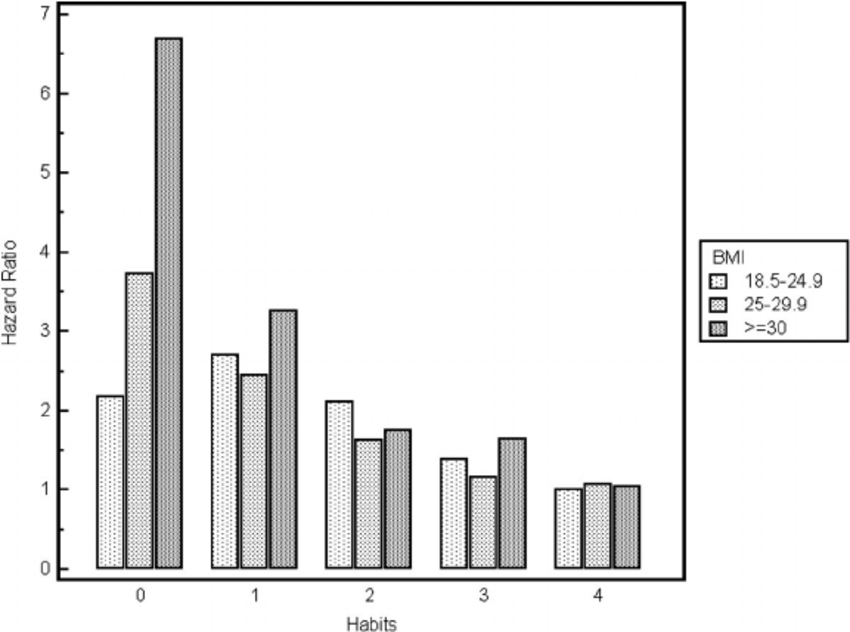
This graph from a papers exploring a weight neutral approach/inclusive approach to reducing health risks using exercise.
Exercise regardless of weight loss has also been shown to reduce mortality rates and improve health regardless of weight. Exercise supports blood pressure, cholesterol, and glucose levels.
Intuitive Eating as Healthy Behaviour
Intuitive eating, a non diet approach to eating, has got over 150 science papers giving us research showing how is supports our physical and mental health. Reduced cholesterol, improved blood sugar control, lower blood pressure are all things that the evidence shows us as well as the reduced incidence of eating disorders. Intuitive eating also may give us higher self-esteem, better mental health, and reduced stress and anxiety. It promotes body acceptance and reduces the negative emotional impact of dieting.
Not only that. Intuitive eating is also a healthy behaviours that is actually sustainable. People who practice intuitive eating are more likely to maintain balanced and varied diets over the long term. This approach fosters a healthy relationship with food, leading to better dietary quality without the need for restrictive eating patterns. Research seen in Appetite (2015) found that intuitive eating was associated with a higher intake of fruits and vegetables and a more consistent eating pattern compared to those who diet.
Healthy Behaviours and Health Regardless of Weight
One study of over 11000 people showed that having healthy behaviours, defined as the habits physical activity, not smoking, not drinking alcohol, eating 5 fruit and vegetables a day has an impact of risk of dying in general, regardless of weight as shown by the graph below.
Its important to note that because these “habits” or healthy behaviours are here, doesn’t mean it is a rule you need to follow them. We need to hold that there are barriers to healthy behaviours which include health itself, ablism, classism, racism, anti fatness , homophobia, transphobia and all these things impact a persons ability to access healthy behaviours. That is not the individual’s responsibility. It is for us to know this and do things in our power to help remove those barriers to health which is where Health at every size does come in.
We must also hold at the same time that we do not have power over health like diet and wellness culture tells us. Unfortunately, steaming our vulvas with herbal remedies and shotting apple cider vinegar in the morning does not guarantee we will live to 100 and be able bodied until then. It also is not a moral failing if we become disabled. Unfortunately/fortunately, bodies body regardless of what we do.
OK so what next?
You’ve read my blog on diets and this one and you want to know where to go with it? I have a list of more resources that are free to tap into anti diet, fat liberation wise (I know a hyperfocus when I see one).
Other wise I have a paid membership that has the most wonderful community with anti diet and nutrition trainings. But also, here is my freebie to continue your curiousity over anti dieting with no intentional weight loss expectations.